Sleeve Gastrectomy Near Baltimore, Maryland
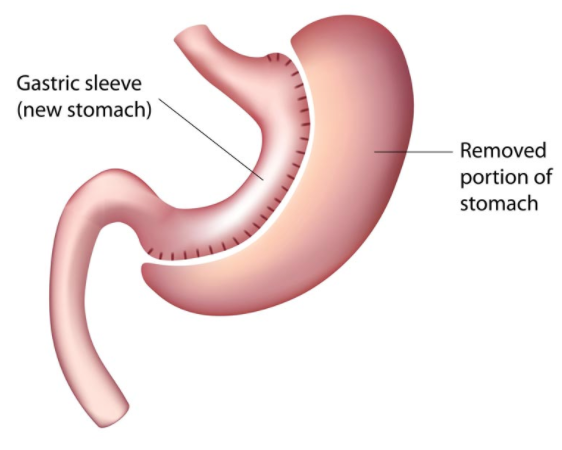
The Sleeve Gastrectomy – often called the vertical or Gastric Sleeve – is performed by removing approximately 80 percent of the stomach. The remaining stomach is a long, slender pouch that resembles a sleeve-like tube. The stomach capacity is greatly reduced, leaving you feeling full after eating only a small portion, which results in weight loss. This makes gastric sleeve surgery in Maryland a highly effective option for patients seeking significant, sustained results. No other part of the intestine is altered with this procedure, preserving the anatomy of the digestive system. As with the gastric bypass, sleeve gastrectomy is performed laparoscopically, and Drs. Averbach, Hamdallah, and Swift will work with you to see if this option is right for you.
Our surgeons hold prestigious medical degrees and have undergone extensive training to ensure the highest level of care.
Understanding Sleeve Gastrectomy
Sleeve gastrectomy, also known as gastric sleeve surgery, is a type of bariatric surgery that involves removing a significant portion of the stomach, leaving a narrow “sleeve” or tube-like stomach. This procedure is designed to reduce the size of the stomach, limit the amount of food that can be consumed, and promote weight loss. Sleeve gastrectomy is a minimally invasive surgery, typically performed laparoscopically, which means it requires only small incisions and a shorter recovery time compared to traditional open surgery.
The Bariatric Sleeve Surgery Procedure Near Baltimore, Maryland
This sleeve gastrectomy procedure works in two ways. First, the new stomach holds a considerably smaller volume than the normal stomach and helps to significantly reduce the amount of food (and thus calories) that can be consumed. The surgery also affects gut hormones that control hunger, satiety, and blood sugar control. A successful weight loss journey requires a lifelong commitment to ongoing support and engagement before, during, and after the surgical process.
Perhaps the greatest advantage of the gastric sleeve lies in the fact that it does not involve any bypass of the intestinal tract, avoiding the chance of intestinal obstruction. It also makes it a suitable form of surgery for patients who previously had bowel resection or are already suffering from Crohn’s disease and a variety of other conditions that would place them at high risk for surgery involving intestinal bypass.
For patients with a particularly high body mass index (typically 50+), many forms of weight loss surgery are either difficult to perform or present increased risk. As a result, vertical sleeve gastrectomy is sometimes performed as the first of a two-part weight loss procedure – Duodenal switch.
For obese patients with a relatively low body mass index, the vertical sleeve gastrectomy can also prove a good choice, especially where existing conditions (such as anemia or Crohn’s disease) prevent them from having other forms of bariatric surgery. In addition, patients may choose this form of surgery if they are concerned about the long-term effects of bypass surgery.
Advantages
- Low mortality rate (0.1%)
- Preservation of normal continuity of GI tract
- Depending on starting BMI, patients typically may achieve weight loss comparable to that of gastric bypass and exceeding adjustable gastric banding
- Reduced risk of nutritional deficiencies
- No risk of marginal ulcer or intestinal obstruction
- Possible in patients with contraindications to Gastric bypass or Duodenal switch.
Disadvantages
- Low mortality rate (0.1%)
- Preservation of normal continuity of GI tract
- Depending on the starting BMI, patients typically may achieve weight loss comparable to that of gastric bypass and exceeding adjustable gastric banding.
- Reduced risk of nutritional deficiencies
- No risk of marginal ulcer or intestinal obstruction
- Possible in patients with contraindications to Gastric bypass or Duodenal switch
Prevention of Reflux/GERD after Gastric Bypass (Gastric Sleeve)
Morbidly obese patients prior to bariatric surgery suffer from a higher frequency of reflux symptoms compared to the general population. To minimize the risk of significant GERD after bariatric surgery, we actively screen patients for symptoms of reflux and hiatal hernia. If detected, we repair it during the bariatric procedure. This approach minimizes the risk of possible delayed surgery for this condition and greatly improves their quality of life after bariatric surgery.
Prevention of Gall Bladder Disease after Bariatric Surgery
Morbidly obese patients are known to have a higher frequency of Gallbladder disease both prior to and after bariatric surgery compared to the general population. Asymptomatic gall stones can cause acute inflammation with significant weight loss after bariatric surgery in 30-40% of patients. It is our policy to actively screen patients for gall bladder problems prior to surgery and if anything is detected (gall stones, chronic cholecystitis due to dyskinesia, cholesterol polyps), removal of the gall bladder at the time of main bariatric procedure might be recommended. Consequently, risk of repeat surgery for gall bladder surgery later on is avoided. If no problems with the gall bladder are detected, after bariatric surgery patients are treated with Ursodiol or Actigall for first six months after bariatric surgery to prevent problems with the gall bladder.
Get started today! Click here to view our online weight loss surgery seminar. The first step in your journey towards a new you!
FAQs About Bariatric Sleeve Surgery
How much does a gastric sleeve cost?
The average cost of gastric sleeve surgery depends on a wide variety of factors, insurance being an important one. If you want to get an estimate of how much gastric sleeve surgery will cost you, schedule a consultation with us, and we’ll give you an accurate cost estimate.
How long does gastric sleeve surgery take?
The gastric sleeve procedure takes a few hours and is done laparoscopically. Patients typically stay in the hospital overnight after the procedure, and most patients are allowed to go home the next day after they’ve been observed.