
Comprehensive Guide to Hernia Repair with Surgical Mesh: An Overview
Hernia repair with surgical mesh: an overview is a widely used technique to fix hernias and reduce the likelihood of them coming back. Surgical mesh is a medical device used in hernia repair procedures to provide additional support to weakened or damaged tissue. This blog offers an overview of the procedure, including the purpose of using surgical mesh, different types of mesh, and the potential benefits and risks. By learning about these aspects, you’ll be better prepared for discussions with your healthcare provider.
Key Takeaways
- Hernias occur when an organ protrudes through a weakened area in muscle or tissue, with common types including inguinal, umbilical, and ventral hernias, often requiring surgical intervention to prevent complications.
- Most hernia repair surgeries are performed using surgical mesh, which has become standard practice to reduce recurrence rates.
- Surgical mesh is a critical component of hernia repair, categorized into synthetic, biological, and composite types, each with distinct characteristics affecting their suitability for specific patient conditions and surgical techniques.
- Advancements in surgical mesh technology and techniques, including drug-loaded meshes and minimally invasive surgical options, aim to enhance patient outcomes, reduce complications, and facilitate quicker recovery post-surgery.
Understanding Hernias
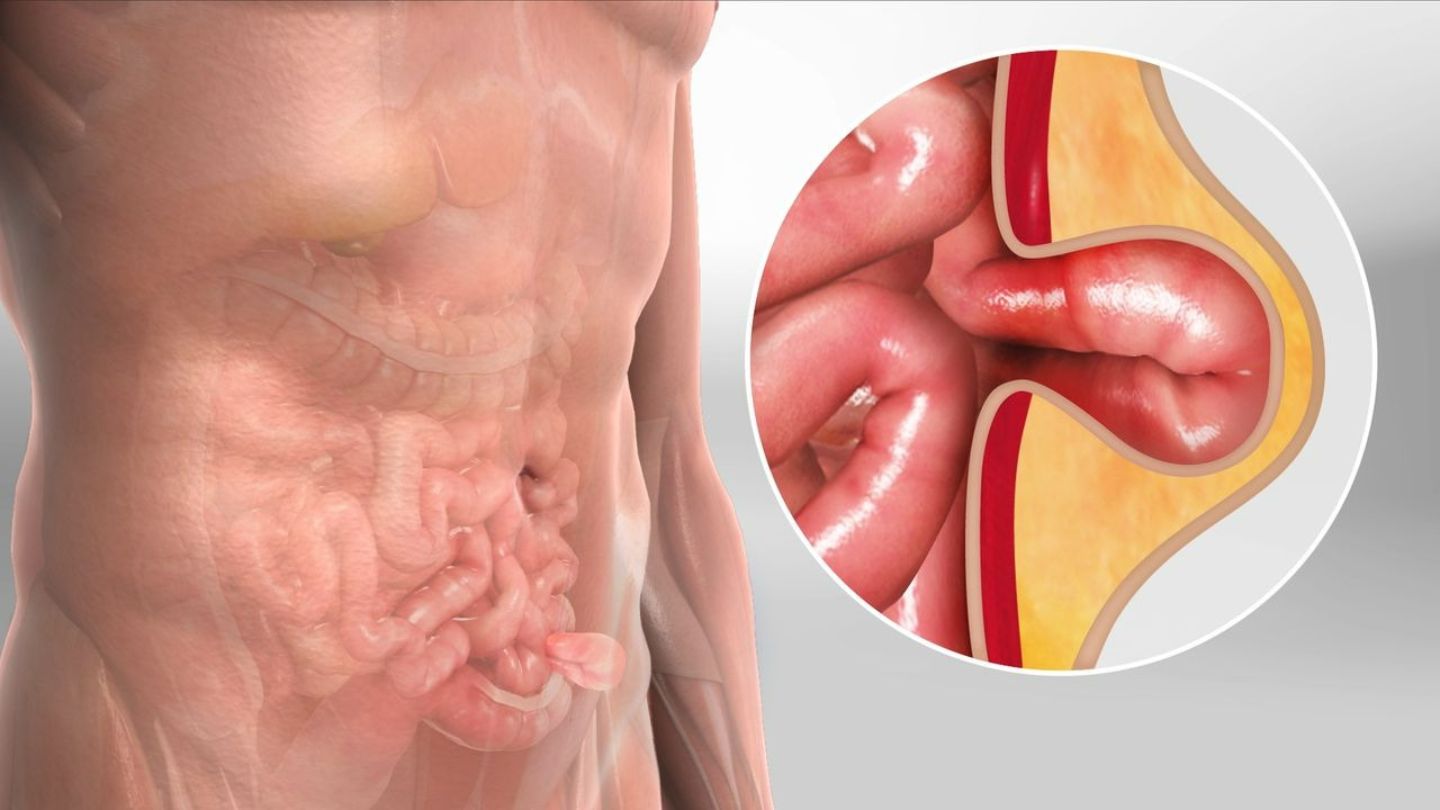
Hernias are characterized by the protrusion of abdominal organs through a weakened area in the muscle or tissue that usually holds them, often resulting in noticeable lumps. This condition can occur in anyone and is categorized into several types. A hernia defect refers to the anatomical weakness or opening in the abdominal wall that allows organs or tissue to protrude.
The most common hernia varieties include:
- Inguinal hernias, constituting around 75% of all cases, are predominantly seen in men
- Umbilical hernias
- Femoral hernias
- Hiatal hernias
- Congenital diaphragmatic hernias
- Incisional hernias
-Ventral Hernia
While some individuals with a hernia may experience symptoms such as bulging, pressure, or discomfort during physical exertion, others might not exhibit any signs until more serious complications emerge. Early detection is crucial for avoiding significant health problems later on. Abdominal wall repair is often required for complex ventral hernias to restore the integrity of the abdominal wall.
Factors contributing to an increased risk of developing a hernia can range from engaging in heavy lifting or persistent coughing to obesity and previous abdominal surgeries, all potentially elevating intra-abdominal pressure and precipitating muscular weaknesses.
Ignoring a hernia could lead to its progressive deterioration, with time potentially causing dangerous conditions like incarceration or strangulation of an organ’s blood supply—a scenario requiring prompt intervention due to the increased risks for severe pain and life-endangering outcomes, hence immediate diagnosis & management are necessary. Surgical treatment is often necessary to prevent complications from hernias.
Inguinal hernia is one type that frequently necessitates surgery, which underscores the importance of finding reliable treatment modalities. Ventral hernias that appear within the abdominal wall are notoriously difficult to remedy and may require elaborate surgical procedures for proper repair.
Repair surgeries for hernias target repositioning misplaced organs back in their rightful place while strengthening weak spots as a measure against incidents. The goal of surgery is to repair hernias and reinforce the affected area. This goal is aided by employing a healthy material for tissue reinforcement, which significantly lowers the chances of subsequent occurrences and emphasizes the role of surgical mending services in treating herniated issues.
We will delve deeper into how surgical mesh gets incorporated in the context of hernia repair, the wide array of types available, and the features that tend to be beneficial. Surgical mesh is used to support damaged tissue and reinforce the abdominal wall during hernia repair. In gaining insights into these processes, you’ll better comprehend the multifaceted nature of hernia treatment strategies and an enhancement that facilitates a more positive result for those affected.
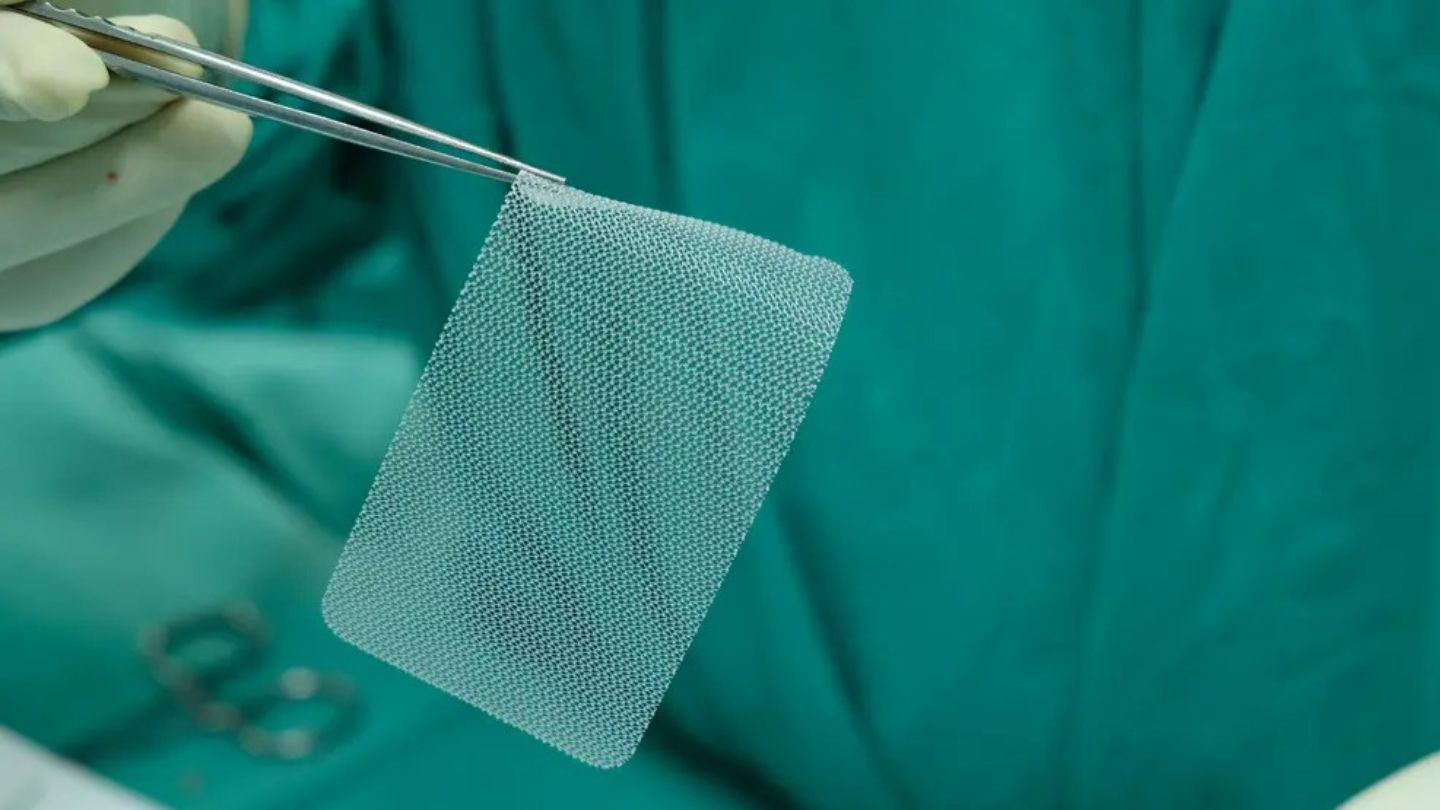
Surgical Mesh in Hernia Repair
Surgical meshes, including prosthetic mesh, hernia mesh, and various hernia meshes, are utilized to bolster tissue in hernia repair operations, offering additional support where tissues have weakened. Mesh implantation initiates a biological response, including inflammation and tissue integration, which is critical for mesh repair success. Due to their efficacy in ensuring durability over time and decreasing the likelihood of a hernia returning, these materials have become the preferred choice for such procedures. They act as frameworks that not only fortify but also encourage new tissue growth at the site of repair.
There are two main types of surgical mesh: synthetic and biological. Most synthetic meshes are typically made from synthetic material such as polypropylene (PP meshes), polyethylene terephthalate (PET meshes), or other polymers, which, while strong, can incite inflammation and adhesion complications. Lightweight meshes, with larger pores and thinner filaments, are designed to reduce foreign body reaction and improve tissue integration. Permanent meshes, made to remain in the body indefinitely, have been widely used but are associated with long-term complications such as infection and tissue growth issues, prompting interest in bioresorbable and nonpermanent alternatives. Dual mesh and composite meshes combine multiple materials to minimize adhesions and support tissue ingrowth. Woven mesh and knitted meshes, constructed from individual mesh fibers, differ in their interlaced or knitted structures, influencing mesh properties like mechanical strength, pore size, and elasticity, which affect clinical outcomes. Biological meshes are derived from animal tissue, such as porcine or bovine sources, and are processed to create absorbable devices that promote tissue integration and reduce infection risk. The decision between using a synthetic or biological mesh is dependent on individual patient cases, along with how complex their hernias may be.
Combining features of both categories leads us to hybrid meshes—dual systems engineered to harness filament mechanical strengths characteristic of synthetics, yet enhance bodily integration similar to biologics, aiming at mitigating adverse effects.
The strategic placement during implantation plays an essential role in ensuring successful outcomes after hernia surgeries. Mesh implantation not only provides a durable closure but also triggers a cascade of biological processes, including inflammation, tissue reaction, and scar tissue formation. Minimally invasive techniques such as laparoscopic or robotic surgery help shorten recovery durations, along with reducing discomfort post-surgery by enabling precise positioning necessary for ideal ingrowth, leading to sustained repairs. Meshes must be able to withstand maximum intra-abdominal pressure, such as 170–180 mmHg generated during coughing or physical activity, to prevent failure.
Meshes find particular use when dealing with common conditions like inguinal or ventral hernias—in inguinal cases, they might reinforce part of the abdominal wall called the posterior rectus sheath, while occasionally necessitating full abdominal wall reconstructions. Ventral repairs tend towards complexity contingent upon defect size plus location specifics.
Nevertheless, inserting any foreign material carries inherent risk factors, including potential reactions against the introduced fabric. The body recognizes the mesh as a foreign body, which can trigger a foreign body reaction involving immune cells and chronic inflammation. This can lead to mesh shrinkage, which negatively impacts long-term outcomes such as recurrence and tissue integration, and may require corrective interventions. Tissue reaction, including fibrosis and scar tissue formation, is part of the healing process and influences mesh stability and integration.
Delving deeper helps clarify impacts surrounding different mesh varietals plus qualities over success rates within the realm of continuous evolution targeting “perfect” interlacing capable of delivering required reinforcement, meanwhile fostering healthy healing, curbing complication odds. Mesh properties such as mechanical strength, pore size, and elasticity are critical in determining performance, tissue response, and postoperative outcomes. The structure of individual mesh fibers, as well as whether the mesh is a knitted mesh or woven mesh, influences tissue reaction, infection risk, and overall clinical results. Host tissue colonization and the formation of new blood vessels are essential for mesh integration and healing. Collagen deposition and the formation of new connective tissue at the repair site further strengthen the repair and promote long-term success.
Types of Surgical Mesh
Various types of surgical meshes are available, each with distinct characteristics and intended uses. There are primarily three categories: absorbable mesh, non-absorbable mesh, and composite meshes. It is essential to discern the differences between these types for optimal selection in hernia repair surgery.
Absorbable meshes gradually deteriorate over time until they fully integrate into the body’s tissues. These types of meshes are often utilized in areas that might be contaminated to reduce infection risks. Their limited structural integrity can lead to a disadvantage, increased risk of hernia recurrence as the material breaks down.
In contrast, non-absorbable meshes provide enduring stability and meet high mechanical demands due to their construction from synthetic materials like polypropylene. They remain permanently within the body after implantation. Despite offering resilience over time, potential issues such as rigidity or complications related to erosion and tissue adhesion may arise with their use.
Composite meshes offer an integrated solution by marrying both absorbable and non-absorbable components, aiming for immediate postoperative support while mitigating long-term complication risks associated with permanent implants – thereby leveraging advantages from both absorbable and non-absorbable mesh traits.
Biological surgical options exist in forms derived either allogenically or xenogenically that align closely with human tissue, facilitating natural growth around existing host cells, though typically present lower tensile strength than synthetics, leading potentially to higher rates of recidivism upon application.
Factors influencing which type of mesh is selected include patient-specific considerations, the complexity inherent in individual cases, and surgeon preference informed by experience levels, among other factors, e.g., deploying synthetic variants for simpler low-grade presentations versus biological alternatives reserved for complex instances where circumstance dictates necessity accordingly.
Unpacking these key attributes underlying various surgically implanted fabrics clarifies that choosing appropriately involves consideration across multiple dimensions—to secure an option providing sufficient durability coupled favorably biocompatible qualities all conducive toward fostering successful integrative response resulting ultimately enhance quality results following operationally executed interventions aimed at correcting respective conditions effectively thus elevating overall beneficiary satisfaction, relatively speaking.
Key Properties of Surgical Mesh
The success of hernia repair surgeries is greatly influenced by the mechanical attributes of surgical mesh, such as its flexibility and capacity to withstand tension. These qualities are essential for ensuring that the mesh performs effectively during and after surgery by replicating the natural tension of the abdominal wall and supporting recovery.
Considering mesh weight is critical. Heavier meshes can bear more force but may cause increased rigidity and discomfort compared to their lighter counterparts. Lighter-weight meshes tend to be associated with reduced post-surgical pain and a diminished inflammatory response. Thus, they are often preferred by surgeons.
Pore size within surgical meshes also has an impact on their effectiveness. Meshes designed with larger pores allow for improved tissue integration and lower infection rates in contrast to those with smaller pores, since large pores aid connective tissue growth, which strengthens stability while enhancing compatibility with body tissues.
Mesh design plays a pivotal role in terms of biocompatibility and healing efficacy post-implantation. Utilizing monofilament materials when constructing meshes can promote better incorporation into surrounding tissues while limiting inflammation, proving crucial for superior tissue fusion over time as well as long-term durability.
Composite meshes incorporate absorbable components that dissolve over time along with non-absorbable elements, offering an advanced solution especially suited for minimizing adhesions when used inside the peritoneal cavity during hernia repairs.
Choosing an ideal mesh necessitates evaluating tensile strength alongside porosity level, plus overall mass tailored toward individual patient requirements—it involves identifying not just robustness but rather attaining optimal harmony among these properties relative to specific patient circumstances, coupled with chosen operative techniques involved in repair surgery.
Finally, we will delve into various surgical methods involving use of mesh examining how these features factor into achieving positive outcomes from hernia repair operations—recognizing this relationship between properties inherent in different types of available surgical meshes combined within varying techniques stands vital towards securing effective recoveries hence promoting favorable results amongst patients following interventions aimed at mending hernias.
Surgical Techniques Using Mesh
Several methods are available for hernia repair surgery, each offering unique benefits and considerations. These primary surgical techniques include open repair, laparoscopic, and robotic surgeries. The selection among these approaches depends on factors such as the size of the hernia, its complexity, and the surgeon’s skill level.
The traditional approach to hernia repairs is through open repair surgery, which involves making a significant incision to expose the affected area. This method is especially useful for addressing large or intricate hernias due to its comprehensive visibility and access during the procedure. Patients may face extended recovery periods and more considerable scarring with less invasive strategies.
Laparoscopic surgery utilizes minimal invasiveness by employing tiny incisions along with a camera inserted through a small opening to navigate surgical tools during treatment procedures. This technique uses a small incision to access the surgical site. Advantages include diminished postoperative discomfort, shorter convalescence durations, and reduced scarring.
Advancements in minimally invasive methods have led us toward robotic surgery that uses state-of-the-art technology, enabling precise maneuvers alongside improved visualization capabilities throughout surgical interventions related specifically to robotics-aided repairing of damage. Minimally invasive surgery often involves multiple small incisions, resulting in less tissue damage and faster recovery. This contributes to potentially lower levels of bleeding, lesser scar formation, and decreased recuperation times, although typically extending duration itself relative to classic openly conducted operations.
Mesh choice correlates directly with the types utilized, where lighter meshes tend to be preferred when dealing with cases requiring minimal intrusiveness, given their adaptability, coupled with lowered chances of subsequent patient pain. Mesh features like density and pore sizes are critical contributors ensuring proper integration into surrounding tissues, maintaining long-standing stability.
Implanting surgically based frameworks remains a vital aspect that determines the overall success rate expected within the context. Relying on both laparoscopic and robot-assisted methodologies permits detailed, accurate placements of the mesh using specialized surgical instruments, thereby enhancing the likelihood of success regarding respective undertakings.
Patients who undergo robotically facilitated fixes can expect resumption of normal activities shortly after mere matter days post-operation, with substantial benefits for those leading active lifestyles needing quickened returns to employment duties alike.
Crucially understanding impacts arising from different selections regarding operative routes combined with implications inherent in varying components applied (such as mesh properties, etc.) proves pivotal, contemplating the aftermath of possible issues encountered, all ultimately striving towards realizing endeavours successfully, effectively improving beneficiary outcomes whilst simultaneously attempting to ensure minimal chance of reoccurrence problems later down the line…
Postoperative Considerations
Following hernia repair surgery, individuals may face a range of complications, such as:
- ongoing pain
- infection
- blockages in the bowels
- movement of the mesh from its original placement
Postoperative pain is a common complication after hernia repair and can be influenced by factors such as the type of mesh used and the surgical technique applied.
It is essential to vigilantly monitor for these issues to facilitate prompt treatment and mitigate additional problems.
In some instances, contraction or erosion of the mesh can transpire, potentially prompting another surgical procedure if it becomes severe. Indicators that the body might be rejecting the mesh include inflammation around the area, sensitivity to touch, and symptoms similar to those experienced during illness. Early detection of these signs is vital for effectively handling any arising difficulties.
A bowel obstruction represents a grave complication after a post-hernia repair operation. Symptoms often involve an inability to expel gas or feces along with discomfort in the abdomen. Immediate medical care should be sought after encountering such symptoms so as to not only treat this condition but also prevent dire outcomes.
Persistent infections following procedures involving mesh can provoke marked swelling within tissue structures and could necessitate removal operations regarding said meshes. Rigorous after-surgery attention, along with vigilant supervision, is paramount in recognizing and confronting infections without delay.
Addressing pain following an operation remains fundamental during recuperation periods. Less invasive approaches like laparoscopic techniques or robotic-assisted surgeries have been correlated with lesser degrees of pain following procedures when juxtaposed against more conventional open methods utilized during repairs.
Chronic pain can develop after hernia repair and may significantly impact a patient’s quality of life.
Implementing efficacious strategies aimed at controlling discomfort serves dual purposes: they improve patient outcomes while simultaneously improving their convalescence quality, particularly significant among chronic sufferers enduring consistent agony.
Patients benefitting from robotic-assisted hernia restoration typically experience abbreviated recovery durations coupled with swifter reinstatements concerning routine activities—a considerable merit which allows patients less interruption while resuming everyday life schedules post-operatively.
Investigations into pioneering developments related specifically to hernial restorative meshes uncover objectives concentrated on decreasing operational aftermaths. Enhancing patient prosperity stands central amidst ambitions striving towards carrying out corrective measures, boasting low relapse likelihoods, and ensuring overall enhanced health statuses.
Innovations in Hernia Repair Mesh
Progress in the technology of hernia repair meshes is consistently enhancing outcomes for patients and reducing complications. A significant breakthrough has been the introduction of meshes impregnated with drugs that dispense medicinal substances after surgery, aiming to accelerate healing, cut down on infection risks, and bolster overall success rates of surgeries.
Advancements are also being made in creating mesh designs that encourage ideal integration with bodily tissues and exhibit superior compatibility. These innovative steps involve integrating novel materials into their design to diminish issues such as shrinkage of mesh material, erosion, or adverse tissue reactions to foreign objects.
Innovation extends to hybrid meshes that meld synthetic with organic materials. The intention behind these hybrids is to leverage the strength inherent in synthetics while fostering improved connection with connective tissues – all this is aimed at curtailing complication chances.
By harnessing cutting-edge production techniques, it’s now possible to craft specialized meshes characterized by exact pore sizes and mechanical attributes aligned closely with individual patient necessities. Such bespoke solutions have shown promise in boosting efficacy across hernia repair procedures and subsequently improving results for patients.
Likewise, revolutionary surgical approaches like robotic assistance and laparoscopic interventions are contributing. These minimally invasive strategies not only allow precise placement but also limit potential complications, facilitating a smoother recovery process along with more favorable long-term results post-surgery.
When deliberating over an appropriate mesh selection for repairing a hernia, factoring technological advancements becomes crucially important. Surgical practitioners who choose optimally compatible meshes paired with refined procedural methods greatly increase the likelihood of successful procedures while minimizing recurrence risks.
Read more: What is laparoscopic incisional hernia repair: What You Need to Know
Choosing the Right Mesh for Hernia Repair
When selecting a mesh for hernia repair surgery, various factors need to be carefully assessed. The particular clinical situation and the desired results are central to making an informed decision. Surgeons must take into account the type and severity of the hernia, as well as the patient’s health status and any potential risks that may affect mesh selection.
There are distinct benefits and drawbacks associated with both synthetic and biological meshes. Synthetic options like PP mesh offer robust support but can trigger inflammatory responses, while biological variants made from natural tissues aim for integration with the body to minimize infection risk. Determining whether to use synthetic or biological types—and potentially a prosthetic option—depends on each patient’s condition, along with specific surgical requirements.
For placements within the peritoneal cavity, preventing adhesion formation is paramount. Hence, preference might be given toward lightweight meshes with larger pores that promote tissue incorporation while reducing complications after surgery. Composite meshes present an intermediate solution by blending absorbable materials for short-term effectiveness without long-term repercussions.
A surgeon’s expertise plays an indispensable role in choosing an appropriate mesh by examining its mechanical characteristics, compatibility with living tissues, and overall design relevance, which must coincide not only with chosen surgical methods but also adapt finely to individual patients’ needs.
Advanced techniques such as robotic-assisted or laparoscopic surgeries dictate their own criteria regarding suitable properties of surgical mats, including flexibility for ease of placement through minimally invasive procedures aimed at expediting healing times alongside minimizing postsurgical issues leading to faster recoveries.
In essence, determining which surgical mat is ideal requires a comprehensive understanding across multiple domains involving intricate details about both patient profile specifics combined seamlessly against backdrop knowledge concerning various available mats, accompanied astutely throughout by seasoned judgement from experienced surgeons, all culminating harmoniously towards maximizing prospects commensurate with success rates, thereby enhancing overall prognosis post-hernia repair interventions.
Moving Forward with Confidence in Hernia Care
Understanding hernia repair with surgical mesh provides valuable insight into one of the most common yet crucial procedures in modern surgery. From identifying hernia types and risks to selecting the most appropriate mesh and surgical technique, the process is multifaceted and must be tailored to each individual. Advances in mesh technology and surgical methods, such as laparoscopic and robotic-assisted procedures, continue to improve patient outcomes, reduce complications, and speed up recovery times. Choosing the right approach, under the guidance of a skilled medical team, is key to achieving long-lasting results and minimizing recurrence.
If you are considering hernia repair in Baltimore, trust the team at Ascension Saint Agnes Bariatric Surgery to guide you through the process with expert care and advanced treatment options. As part of our commitment to your well-being, we combine state-of-the-art technology with compassionate, individualized support. Whether you’re dealing with a complex case or exploring minimally invasive techniques, we’re here to help you make informed decisions and get back to your best self—faster and stronger. Let us be your partner on the journey to better health and renewed confidence.
We also offer specialized procedures, including laparoscopic primary/incisional hernia repair, treatment for gerd after gastric sleeve, and the endoscopic gerd/reflux procedure, ensuring comprehensive care tailored to your specific needs. Contact us to be your partner on the journey to better health and renewed confidence.