Laparoscopic GERD Reflux/Hiatal Hernia Repair Near Baltimore, Maryland
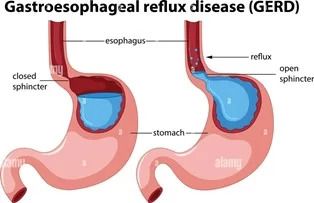
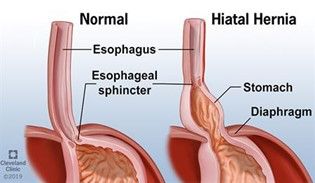
Gastroesophageal reflux disease is a widespread condition presenting with heartburn, regurgitation, hoarseness, and pain or difficulty with swallowing food. It is a result of dysfunction of the normal valve mechanism at the junction of the esophagus and stomach, and many patients seeking care for GERD reflux in Baltimore also have some degree of hiatal hernia. When the stomach is displaced into the chest, it can cause nausea, vomiting, pain after eating, regurgitation of food, or progressive inability to swallow food. Additionally, 10-15% of bariatric patients suffer from reflux symptoms frequently associated with hiatal hernia that were not addressed during their initial bariatric procedure, recurred, or developed after weight loss. These reflux symptoms can affect the quality of life and do not always respond to medical therapy with antacids. If left untreated, GERD can lead to complications such as esophagitis, stricture, and Barrett’s esophagus, a condition where the esophageal lining changes due to prolonged acid exposure, increasing the risk of esophageal cancer. Depending on the clinical situation, GERD reflux can be addressed with a few different procedures.
Dietary changes are crucial in managing GERD symptoms. Modifying food intake, such as reducing acidic and fatty foods, can significantly help protect the esophagus.
Fundoplication for Gastroesophageal Reflux Disease
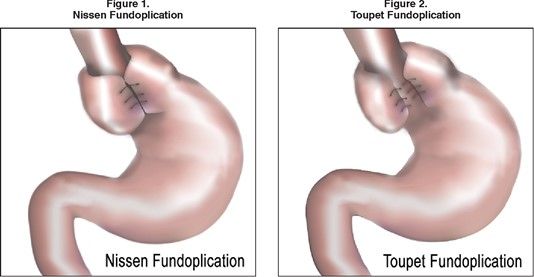
The most common surgery designed to treat GERD and repair the valve mechanism is called a Fundoplication and is combined with a hiatal hernia repair. This procedure consists of the reduction of the herniated junction of the esophagus and stomach into the abdomen with the closure of the diaphragm muscle defect to keep the stomach in the abdomen. The top of the stomach is then wrapped around the esophagus to recreate the valve. Our expert medical team performs a partial or toupet fundoplication, which has fewer significant side effects compared to the more widely known complete Nissen fundoplication.
A fundoplication may be an option for you if:
- You have significant reflux that is not responsive to medication therapy
- Have a large hiatal hernia
- Have a desire to stop taking your antireflux medication
Advantages
- Low mortality rate
- Ability to address large hiatal hernia at the same time
- High rates of reflux remission
- The procedure has a long history with well-established clinical outcomes
- Three different degrees of wrap so they can be personalized to your particular situation
Disadvantages
- Not able to be performed on patients who have had a sleeve gastrectomy or duodenal switch
- Difficult to perform on patients who have undergone a roux gastric bypass
- Possibility of recurrence
- Higher rates of gas bloat, dysphagia, and flatulence rates of gas bloat, dysphagia, and flatulence
- Foods that you eat now may cause discomfort, nausea, or vomiting after your surgery due to changes in how stomach acids interact with your digestive system
- Requires adherence to dietary recommendations and follow-up compliance
- Patients with high BMI may need an additional procedure to prevent recurrence
Ascension Saint Agnes Hospital provides expert treatment for GERD reflux. Our experienced team of specialists will work with you to develop a customized treatment plan that fits your needs. Contact us today to learn more about our GERD reflux and other services.
Minimally Invasive Procedures
For certain patients, minimally invasive procedures offer an effective solution for treating acid reflux. Two common procedures are laparoscopic fundoplication and transoral incisionless fundoplication (TIF).
Laparoscopic fundoplication involves making several small incisions in the abdomen to access the stomach. The upper portion of the stomach is then wrapped around the lower portion of the esophagus to strengthen the LES and prevent stomach acid from flowing back into the esophagus. TIF, on the other hand, is a procedure that uses a flexible tube with a camera and instruments to perform the same wrap without external incisions.
Both procedures aim to reduce symptoms of acid reflux and improve the patient’s quality of life. Clinical trials have demonstrated high success rates and low complication rates for these minimally invasive techniques. However, a comprehensive treatment plan, including lifestyle changes and medication, may still be necessary to achieve the best outcomes.
It is essential to discuss the risks and benefits of minimally invasive procedures with a doctor to determine the most appropriate course of treatment for your specific condition.
FAQs About Hiatal Hernia Repair
How long does hiatal hernia repair last?
Ideally, hiatal hernia repair will last a lifetime. However, hiatal hernia recurrences do happen and are generally repaired in the same way the surgery was done initially. In case of recurrence, patients are asked to report it immediately.
How much does hiatal hernia surgery cost?
In order to get an accurate estimate of the cost of hiatal hernia surgery, you’ll need to contact us. We’ll give you an accurate cost estimate, including all relevant fees, and we’ll help you figure out what your insurance will be able to pay.
Can a hiatal hernia come back after surgery?
Hiatal hernia recurrences do happen and, depending on the way the procedure was done, can be common. However, hiatal hernia recurrence typically isn’t much of a worry and can be repaired in a similar way to the surgery that was initially done.
What is the success rate of hiatal hernia surgery?
The success rate of a hiatal hernia surgery, on average, is between 90 and 95 percent. This rate does not include recurrences that happen years after surgery. Many factors impact the success rate of hiatal hernia surgery. We ask that if you have any concerns, schedule a consultation with us.