
Understanding Different Types of Hernias and Their Treatments
Hernias are more common than many people realize, often developing quietly before causing noticeable discomfort or complications. They occur when internal tissue pushes through weakened muscle, creating symptoms that can vary from mild pressure to significant pain. Early recognition and proper treatment are essential for preventing long-term issues. Understanding how hernias form and why they require medical attention helps patients make informed decisions about care. In this blog, we explore the different hernia types and the treatment options available.
Key Takeaways
- Hernias occur when organs or tissues push through weakened areas in muscle walls, with over 800,000 hernia repairs performed annually in the United States
- The six main types include inguinal (most common, affecting 27% of men), femoral, umbilical, incisional, ventral, and hiatal hernias, each requiring specific treatment approaches
- While some hernias can be managed with watchful waiting, most require surgical repair using either open or laparoscopic techniques with mesh reinforcement
- Early recognition of symptoms like visible bulges, pain during straining, and pressure sensations is crucial to prevent serious complications like strangulation
- Risk factors include age over 50, male gender, family history, chronic coughing, heavy lifting, and previous abdominal surgeries
What is a Hernia?
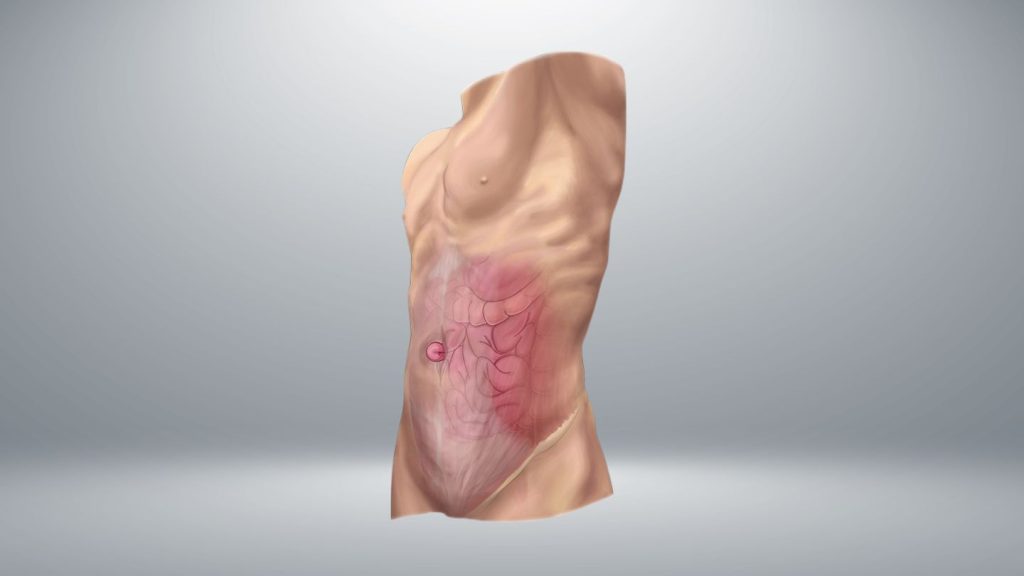
A hernia occurs when an organ, fatty tissue, or part of the intestine pushes through a weak spot or opening in the muscle or connective tissue that normally contains it. Think of it like a tire with a weak spot in the sidewall – when pressure builds up inside, the inner tube can bulge through that weakened area.
Most hernias develop in the abdominal area, where increased pressure can force tissues through weakened muscle walls. The abdominal wall consists of multiple layers of muscle and connective tissue that work together to keep your internal organs safely contained within the abdominal cavity. When these protective barriers weaken due to age, strain, or previous injury, a hernia occurs.
These protrusions create visible bulges that may appear and disappear depending on your body position and activity level. When you’re lying down and relaxed, the hernia bulge often becomes less noticeable or disappears completely. However, when you stand, cough, or strain, increased pressure causes the protruding tissue to become more prominent and potentially painful.
Hernias range from small, asymptomatic protrusions that cause minimal discomfort to large, painful masses requiring immediate medical attention, especially for those wondering if they can safely exercise with a hernia. Understanding the different types of hernias and their treatments empowers you to recognize symptoms early and seek appropriate care before serious complications develop.
Types of Hernias and Their Treatment
Understanding different types of hernias is essential for recognizing symptoms and seeking appropriate medical care, particularly when considering the potential need for hernia repair with surgical mesh. There are six primary types based on location and affected tissues, each with distinct characteristics and treatment requirements. Some types are more common in specific demographics – men, women, infants, or elderly patients – due to anatomical differences and varying risk factors.
Inguinal Hernia
An inguinal hernia is the most common type of hernia, accounting for about 75% of all hernias and affecting 27% of men during their lifetime. This type of hernia occurs when intestinal tissue pushes through the inguinal canal in the groin area near the inner thigh. The inguinal canal is a natural passage in the lower abdominal wall that contains blood vessels and nerves leading to the reproductive organs.
This hernia type is significantly more prevalent in men due to the pathway created when testicles descend through the abdominal wall during fetal development. This descent leaves a natural weak point in the abdominal wall that can become problematic later in life, especially when combined with factors that increase pressure in the abdomen.
Symptoms of an inguinal hernia include a bulge in the groin that may extend into the scrotum in men. You might notice pain when coughing or lifting heavy objects, along with general aching sensations in the groin area. The bulge typically becomes more prominent when you’re standing or straining and may disappear when you lie down.
Treatment for inguinal hernias typically requires surgical repair, as these hernias rarely heal on their own and can lead to serious complications if left untreated. The good news is that inguinal hernia repair is one of the most commonly performed and successful surgeries, with excellent outcomes that often influence expectations regarding recovery time after hernia repair surgery.
Femoral Hernia
Femoral hernias develop when tissue pushes through the femoral canal, appearing as a bulge at the top of the inner thigh below the groin. This type of hernia is more common in women than men, particularly in those over 50 and during pregnancy, due to the wider pelvic structure in women that creates more space in the femoral canal.
These hernias are often smaller than inguinal hernias but carry a higher risk of strangulation due to the tight femoral canal opening. The narrow space through which the hernia protrudes can easily become constricted, cutting off blood supply to the trapped tissue. This makes femoral hernias particularly concerning from a medical standpoint.
One challenge with femoral hernias is that they may be less noticeable than other hernia types, making early detection difficult. The bulge might be small and located in an area that’s not immediately visible, leading to delayed diagnosis. However, you might experience discomfort in the upper thigh or groin area, especially when walking or climbing stairs.
Due to the high risk of complications, femoral hernias require immediate surgical repair even when asymptomatic. Your hernia surgeon will likely recommend prompt treatment to prevent the dangerous complications that can occur when this type of hernia becomes trapped or strangulated.
Umbilical Hernia
An umbilical hernia forms when abdominal tissue protrudes through a weakness in the abdominal wall near the belly button. This occurs at the umbilical ring, where fetal blood vessels once passed during development. The belly button area represents a natural weak point in the abdominal wall that can become problematic under certain circumstances.
In newborns and infants under 6 months, umbilical hernias are extremely common and usually harmless. Many of these childhood hernias resolve naturally by age 2-5 as the abdominal muscles strengthen and the umbilical ring closes completely. Parents often worry when they see a bulge near their baby’s belly button, but most pediatric umbilical hernias require only careful observation rather than immediate intervention.
Adult umbilical hernias are different and affect obese adults, pregnant women, and those with multiple pregnancies. The increased abdominal pressure from pregnancy or excess weight can force tissue through the weakened umbilical ring. Unlike childhood cases, adult umbilical hernias require surgical repair as they do not resolve spontaneously.
In children, umbilical hernia repair is only needed if the hernia persists beyond age 5, becomes larger than 1.5 cm, or causes symptoms. For adults, surgery becomes necessary because these hernias tend to worsen over time and can lead to complications if left untreated.
Incisional Hernia
An incisional hernia develops at the site of previous abdominal surgery, where the surgical incision has weakened the muscle wall. This type of hernia affects 10-20% of patients who have undergone abdominal surgery, typically appearing months to years after the original procedure. Any operation that requires cutting through the abdominal wall can potentially lead to this complication.
The development of an incisional hernia often relates to how well the original surgical wound healed. Risk factors include infection at the original surgical site, obesity, smoking, and conditions that impair wound healing, such as diabetes or poor nutrition. Heavy lifting or straining too soon after surgery can also contribute to incisional hernia formation.
These hernias can range from small protrusions that cause minimal discomfort to large, complex hernias involving multiple organs. In severe cases, a significant portion of the abdominal contents may protrude through the weakened area, creating both functional problems and cosmetic concerns.
Surgical repair is usually necessary for incisional hernias because they typically worsen over time without intervention. The repair may require specialized techniques, especially for large or recurrent hernias. Your surgeon might recommend additional measures to strengthen the abdominal wall and prevent future hernias at the same site.
Ventral Hernia

A ventral hernia occurs along the front (anterior) abdominal wall, including epigastric hernias that develop between the belly button and breastbone. These hernias can develop anywhere along the midline of the abdomen where muscles meet, representing areas of natural weakness in the abdominal wall structure.
Epigastric hernias are a specific subtype of ventral hernia that occur in the upper abdomen. They often contain fatty tissue rather than intestinal contents and may be multiple rather than single defects. Some patients develop several small epigastric hernias along the midline, creating what surgeons sometimes call a “Swiss cheese” pattern of defects.
Initially, ventral hernias are often asymptomatic, causing little to no discomfort. However, as they enlarge over time, they may cause pain and complications. The pain typically worsens with physical activity, coughing, or straining. Some patients describe a pulling sensation or pressure in the affected area.
These hernias are more common in adults than in children, with a higher incidence in those with connective tissue disorders that affect the strength and integrity of the abdominal wall. Treatment depends on the size and symptoms, with larger hernias typically requiring surgical mesh repair to prevent recurrence and restore abdominal wall function.
Hiatal Hernia
A hiatal hernia is a unique type where part of the stomach pushes up through the diaphragm into the chest cavity. This differs from other hernia types because it involves the diaphragm rather than the abdominal wall. The diaphragm is the large muscle that separates your chest from your abdomen and helps you breathe.
There are two main types of hiatal hernia. The sliding hiatal hernia is most common and occurs when the junction between the esophagus and stomach slides up into the chest. The paraesophageal type is more serious and happens when part of the stomach pushes through the diaphragm alongside the esophagus while the junction remains in its normal position.
Hiatal hernias affect up to 60% of people over age 60, though many cases remain asymptomatic and are discovered incidentally during other medical examinations. When symptoms do occur, they typically include heartburn, chronic acid reflux, chest pain, and difficulty swallowing. Some patients also experience regurgitation of food or stomach acid.
Treatment for hiatal hernias ranges from lifestyle modifications and medications to surgical repair for severe cases, with many patients benefiting from early mobility strategies such as walking after hernia surgery. Many patients find relief through dietary changes, weight management, and acid-reducing medications. Surgery becomes necessary when conservative treatment fails or when complications develop that threaten the patient’s health and quality of life.
Moving Forward With Confidence in Hernia Care
Understanding the different types of hernias and the treatments available empowers you to make informed decisions about your health. Whether mild or severe, hernias require proper evaluation to prevent complications and ensure long-term stability. Early diagnosis, personalized treatment planning, and timely surgical intervention can significantly improve outcomes and quality of life.
At Ascension Saint Agnes, we provide advanced, patient-centered solutions for hernia repair in Baltimore, ensuring safe, effective care tailored to your needs. Our team is dedicated to guiding you through every step, from evaluation to recovery, with expertise and compassion. Recognizing related digestive and surgical concerns, such as upper endoscopy, GERD reflux after sleeve gastrectomy, and laparoscopic gallbladder bile duct procedures, can help you better understand the full spectrum of care available. Inspired by our commitment to comprehensive surgical support, we encourage you to take the next step toward better health. Contact us to move confidently toward long-term wellness.
Frequently Asked Questions
Can hernias heal on their own without surgery?
Most adult hernias do not heal on their own and typically worsen over time. Only some umbilical hernias in young children may close naturally. Adult hernias require surgical repair because the muscle defect cannot self-correct.
How long does hernia surgery recovery take?
Recovery varies by procedure. Laparoscopic repairs usually allow normal activity in 1–2 weeks, while open surgery may require 2–4 weeks. Heavy lifting is restricted for 6–8 weeks to protect the repair and ensure proper healing.
What is the difference between open and laparoscopic hernia repair?
Open repair uses one larger incision, while laparoscopic surgery uses small incisions and a camera. Laparoscopic repair often offers faster recovery and less pain, though it isn’t suitable for all hernia types or emergency cases.
Are there any activities I should avoid if I have a hernia?
Avoid heavy lifting, straining, and high-impact exercises that increase abdominal pressure. Walking, light stretching, and swimming are generally safe. Your doctor may recommend specific restrictions depending on the type and severity of your hernia.
Can hernias be prevented if I have a family history?
You can reduce risk by maintaining a healthy weight, avoiding smoking, addressing chronic cough or constipation, and using proper lifting techniques. However, genetics may still predispose some individuals to hernias despite preventive efforts.