Gastric bypass is a major weight-loss surgery that reduces the amount of food one can eat and the amount of nutrition one absorbs. The amount of weight you may lose depends on your diet, exercise plan, and the development of new eating habits.
Read more: How Much Weight Will I Lose After Gastric Bypass Surgery?
Embarking on this weight loss journey requires significant changes in your lifestyle and diet. To ensure you meet your post-surgery weight loss goals, here are some food items to avoid:
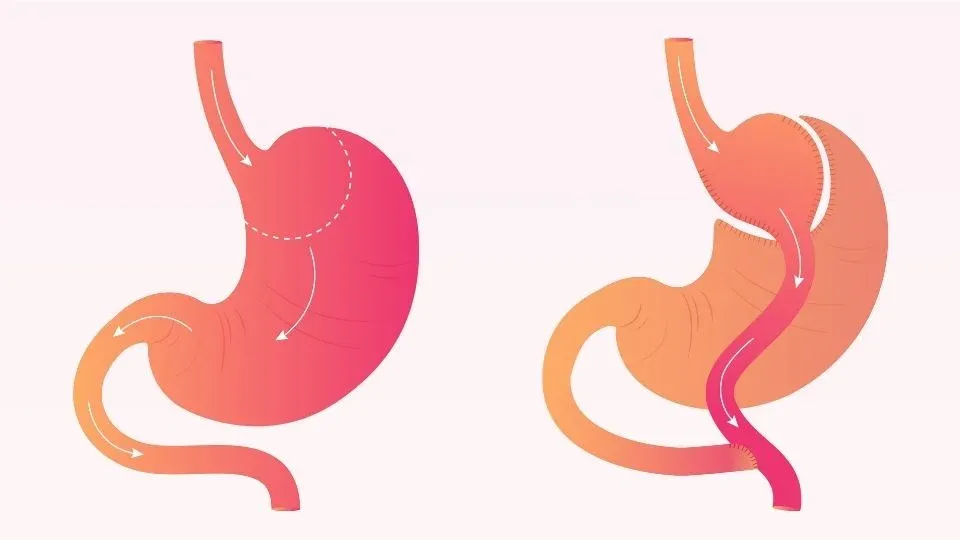
Understanding Gastric Bypass Surgery
Gastric bypass surgery, also known as Roux-en-Y gastric bypass, is a type of weight loss surgery designed to help obese individuals achieve significant weight loss and improve their overall health. This procedure involves altering the digestive system by creating a small stomach pouch and rerouting a portion of the small intestine. As a result, the stomach’s capacity to hold food is reduced, and the body’s ability to absorb nutrients is limited.
The primary purpose of gastric bypass surgery is to assist individuals in losing weight and reducing the risk of obesity-related health issues such as diabetes, high blood pressure, and heart disease. By limiting the amount of food that can be consumed and altering nutrient absorption, gastric bypass surgery can help individuals achieve a healthier weight and enhance their quality of life. This weight loss surgery is particularly beneficial for those who have struggled to lose weight through traditional methods.
Post-Surgery Diet and Nutrition
Importance of a Long-Term Diet after Bariatric Surgery
A long-term diet after bariatric surgery is essential for maintaining weight loss and overall health. Following gastric bypass surgery, the digestive system undergoes significant changes, necessitating a specific diet to ensure proper nutrition and effective weight loss. Adhering to a well-planned diet can help individuals achieve their weight loss goals, prevent weight gain, and minimize the risk of complications.
Typically, a long-term diet after bariatric surgery involves a staged approach, starting with liquids, progressing to soft foods, and eventually incorporating solid foods. It is crucial to work closely with a registered dietitian or nutritionist to develop a personalized meal plan that meets individual nutritional needs and supports weight loss goals. This approach ensures that bariatric surgery patients receive the necessary nutrients while adapting to their new digestive system.
1. High-fat Meats
After your gastric bypass, high-fat meats like bacon, sausage, bologna, and salami should be avoided entirely. Not only are these types of meat fatty and high in calories, but they can also cause digestive issues due to their rich fat content. Eating high-fat meats can lead to more stomach discomfort, ulcers, and diarrhea. Additionally, failing to follow the prescribed eating guidelines and choosing to eat food that is not suitable for post-gastric bypass patients can result in serious complications.
Read more: Can You Eat Popcorn After Gastric Bypass?
2. Sugary Foods
When it comes to bariatric surgery, you must avoid sugary foods. After surgery, transitioning from a liquid diet to solid food should be done gradually to ensure proper nutrition and avoid complications. Sugary foods can spike your blood sugar levels, which can cause weight gain and other health issues. Many of such foods are also high in calories and low in nutritional value. Examples of sugary foods to avoid include candy, cakes, pastries, cookies, ice cream, sodas, and other sugary drinks.
3. Alcohol
Gastric bypass involves a drastic change in how your body absorbs food, and drinking alcohol after the procedure is not recommended. It can be challenging for your body to process the toxins in alcoholic beverages, which could lead to liver damage and serious health risks over time. Additionally, alcohol has a high-calorie content, which can contribute to weight gain if you do not account for it in your daily caloric intake. If you choose to drink alcohol after gastric bypass, you must limit yourself to no more than 1-2 servings per day and avoid high-calorie beverages such as beer or wine coolers.
4. Dry Foods
Dry, crunchy foods are not recommended after gastric bypass surgery because they can be challenging to digest. Dry-roasted nuts, crackers, and pretzels should all be avoided, as these can create a blockage in the stomach or intestine. Additionally, some dry cereals, such as oatmeal, could cause nausea and vomiting if your stomach has not healed completely. Stick to softer, less processed foods that are easier to digest.
5. Caffeinated and Carbonated Drinks
Caffeinated and carbonated beverages should be avoided after gastric bypass surgery. This includes caffeinated coffee or tea, energy drinks, soda, and sparkling water. Caffeine can cause dehydration and increase the risk of dumping syndrome for those who have post-gastric bypass surgery. Carbonated beverages may cause bloating and discomfort.
Read more: Can You Drink Coffee After Gastric Sleeve Surgery?
6. Dairy Products
High-fat dairy products, such as ice cream and cheese, should be avoided after gastric bypass surgery. Dairy products are more likely to cause nausea, vomiting, and dumping syndrome due to their high fat levels. Try to choose low-fat alternatives such as low-fat or non-dairy milk and yogurt. Also, many dairy products are high in sugar, so it is essential to read the nutrition labels carefully.
Conclusion
In conclusion, adapting to a new lifestyle and dietary habits after gastric bypass surgery is vital for achieving long-term weight loss success. By avoiding certain foods and adhering to a structured post-surgery diet, individuals can enhance their weight loss journey and minimize potential complications. Understanding the importance of this dietary discipline is crucial for maintaining the benefits of gastric bypass surgery and ensuring improved health outcomes.
At Ascension Saint Agnes Bariatric Surgery, we specialize in providing comprehensive care and guidance for those seeking Roux-en-Y near Maryland. Our team is dedicated to offering exceptional surgical services with a focus on safety and patient comfort. We offer personalized after-care instructions and support to help you manage lifestyle changes effectively following sleeve gastroplasty or bariatric revision surgery. Contact us today to embark on your weight loss journey with confidence!
FAQs
Can you ever eat normally again after a gastric bypass?
While you can enjoy a varied diet, “eating normally” will be different post-surgery. It’s essential to focus on small, nutrient-rich meals and avoid foods that may cause discomfort or complications.
Can I ever eat pizza again after a gastric bypass?
Pizza can be consumed in moderation if it’s prepared with healthy ingredients. To make it more suitable, opt for a thin crust, minimal cheese, and plenty of vegetables. Always chew food thoroughly and eat slowly.