Roux-en-Y Gastric Bypass Near Baltimore, Maryland
“I had prepared myself for a difficult couple of days after surgery, and what I experienced was the exact opposite; I had no pain. I literally couldn’t believe how great I felt.” – Kim.
The Roux-en-Y Gastric Bypass – often called gastric bypass – is considered the ‘gold standard’ of weight loss surgery and is the second most commonly performed bariatric procedure worldwide. Patients seeking Roux-en-Y in Baltimore, MD, can benefit from a procedure backed by strict bariatric surgery accreditation, which is crucial in ensuring quality and assurance in the field of metabolic and bariatric surgery.
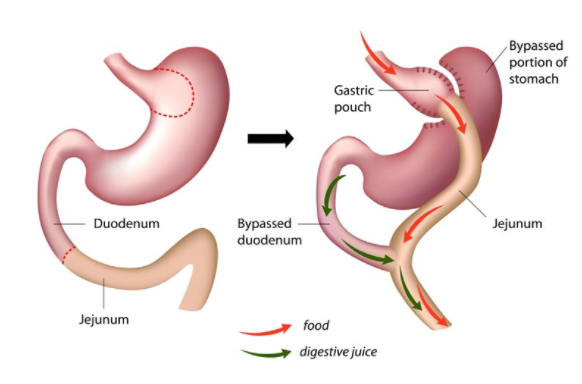
Gastric bypass involves both restrictive and malabsorptive components to produce long-term weight loss. It is restrictive as a result of the creation of a small stomach pouch and malabsorptive because it creates a method for bypassing a variable portion of the small intestine, depending on a patient’s BMI, before surgery.
The Procedure
There are two components to the gastric bypass procedure. First, a small stomach pouch, approximately one ounce or 30 milliliters in volume, is created by dividing the top of the stomach from the rest of the stomach. Next, a Y-shaped section of the small intestine is attached to the pouch, allowing food to bypass the main stomach. Bypassing the two segments of the small intestine, known as the duodenum and part of the jejunum, allows the body to reduce the amount of calories the body absorbs.
The gastric bypass is successful because the newly created stomach pouch is considerably smaller and can only hold a few ounces of food at a time, which translates into fewer calories consumed. There is less digestion of food by the smaller stomach pouch, and the segment of the small intestine that would normally absorb calories no longer has food going through it, so there is less absorption of food. Most importantly, the rerouting of the digestive process produces changes in gut hormones that promote satiety, suppress hunger, and reverse one of the primary mechanisms by which obesity induces type 2 diabetes.
Body mass index (BMI) is a crucial metric in determining eligibility for gastric bypass surgery. It is typically recommended for individuals with a BMI over 40 or between 35 and 40 with related health conditions.
Gastric bypass surgery is performed as a laparoscopic (minimally invasive) procedure that involves the use of a small telescope-like camera inserted through a small incision made in the abdomen, but not everyone is a candidate for this type of surgery.
You and your surgeon can decide together which procedure is right for you.
Advantages
- Low mortality rate (0.2%)
- Weight loss of 65 to 70% of pre-operative excess weight within one year
- Overall improved health
- Improvement or elimination of co-morbidities such as type II diabetes, sleep apnea, hypertension and some others
- Effective weight management strategies and expert guidance to achieve health-related goals and maintain a healthier lifestyle post-surgery
Disadvantages
- Disruption of the staple line can lead to leakage or serious infection
- Possible malnutrition or anemia
- Possible obstruction of the GI tract
- Risk of marginal ulcer
- Risk of dumping syndrome
- Requires adherence to dietary recommendations, life-long vitamin/mineral supplementation, and follow-up compliance
Prevention of Reflux/GERD after Gastric Bypass (Gastric Sleeve)
Morbidly obese patients prior to bariatric surgery suffer from a higher frequency of reflux symptoms compared to the general population. To minimize the risk of significant GERD after bariatric surgery, we actively screen patients for symptoms of reflux and hiatal hernia.
If detected, we repair it at the time of the bariatric procedure. This approach minimizes the risk of possible delayed surgery for this condition and greatly improves their quality of life after bariatric surgery.
Prevention of Gall Bladder disease after Bariatric Surgery
Morbidly obese patients are known to have a higher frequency of gallbladder disease both prior to and after bariatric surgery compared to the general population. Asymptomatic gallstones can cause acute inflammation with significant weight loss after bariatric surgery in 30-40% of patients. It is our policy to actively screen patients for gall bladder problems prior to surgery, and if anything is detected (gallstones, chronic cholecystitis due to dyskinesia, cholesterol polyps), removal of the gall bladder at the time of the main bariatric procedure might be recommended. If no problems with the gall bladder are detected after bariatric surgery, patients are treated with Ursodiol or Actigall for the first six months after bariatric surgery to prevent problems with the gall bladder.
Get started today! Click here to view our online weight loss surgery seminar. The first step in your journey towards a new you!
Frequently Asked Questions About Roux-en-Y Gastric Bypass
How long does it take to recover from Roux-en-Y Gastric Bypass?
Recovering from roux-en-Y gastric bypass is a process that takes several weeks. Patients are given a special post-op diet to assist in recovery. Patients typically are able to return to work after 1-2 weeks post-op. We recommend patients avoid heavy lifting or strenuous activity for 4-6 weeks after surgery.
What can you eat after Roux-en-Y Gastric Bypass? Nutritional Counseling
Patients who get roux en Y gastric bypass are given a special post-op diet that they must follow in order to avoid complications and to kickstart rapid weight loss. Patients start with a liquid fast and are then allowed to start reintroducing pureed and soft foods over time. After about 4 weeks of this diet, patients can start reintroducing normal foods.
Is the Roux-en-Y procedure reversible?
The roux-en-Y gastric bypass is not meant to be a reversible procedure. However, we offer revision surgery to patients who are not satisfied with the results they get from the gastric bypass procedure.
Are there any risks involved in the Roux-en-Y gastric bypass?
Risks involved with the roux-en-Y gastric bypass are minimal; however, most patients will experience some form of abdominal pain. Very few patients will have serious complications resulting from staple line leaks or infections.